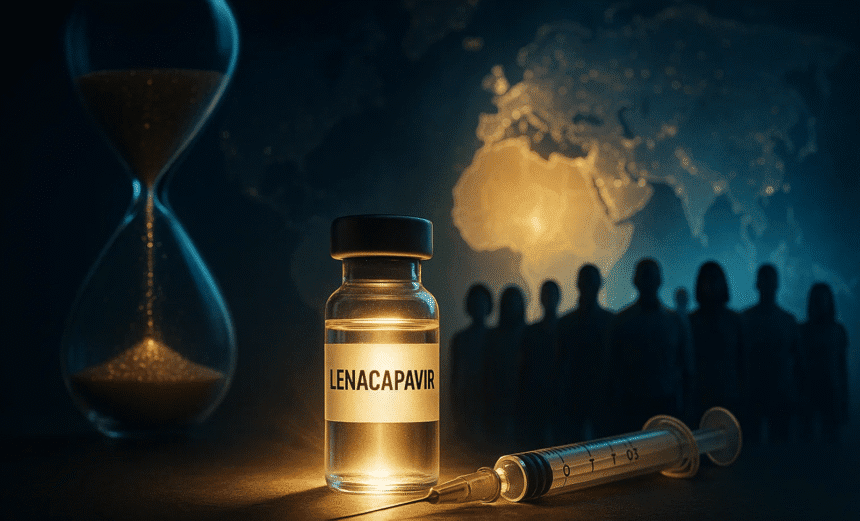
A breakthrough in the global fight against HIV is on the horizon. Generic versions of the twice-yearly injectable drug lenacapavir are expected to be made widely available and affordable by 2027, priced at just US$40 per person per year in around 120 low- and middle-income countries. The announcement was made in late September 2025 by global health partners including Unitaid, the Clinton Health Access Initiative (CHAI), Wits RHI, the Gates Foundation, and Indian manufacturers Dr. Reddy’s Laboratories and Hetero Labs. These partners are working under royalty-free licences granted by Gilead Sciences, the developer of the branded version (Yeztugo). The new agreement is designed to scale up production of the drug and ensure it can reach national HIV programmes through global procurement mechanisms such as the Global Fund.
The promise of lenacapavir lies not only in its affordability but also in its long-acting formulation. Unlike daily oral pills currently used for pre-exposure prophylaxis (PrEP), lenacapavir is administered only twice a year through a simple subcutaneous injection. This feature addresses two persistent challenges in HIV prevention: adherence and stigma. Many at-risk populations struggle to maintain a strict daily pill routine, while others face stigma when seen accessing HIV medication. In pivotal clinical trials, lenacapavir demonstrated remarkable effectiveness, with studies showing it prevented more than 99% of infections among participants when used as PrEP. Experts believe that such a long-acting, reliable option could be a game changer in regions hardest hit by the epidemic.
Globally, the urgency for new prevention tools remains high. By the end of 2024, an estimated 40.8 million people were living with HIV, and 1.3 million new infections were recorded that year alone. While decades of global health campaigns have expanded treatment access and reduced mortality, transmission continues at alarming levels, especially in parts of sub-Saharan Africa and among marginalized groups worldwide. Lenacapavir’s potential introduction in 2027 comes at a critical time: it could accelerate the decline in new infections if rolled out equitably and at scale.
The production and pricing plan for lenacapavir reflects a carefully coordinated partnership. Gilead’s earlier licensing agreements paved the way for generic manufacturing, but the new arrangements offer financial and technical support to expand the supply of active pharmaceutical ingredients (APIs) and establish the infrastructure for large-scale production. With donor backing, the $40 annual cost target represents one of the most affordable long-acting PrEP options ever proposed, making it financially feasible for governments and health agencies to integrate the drug into their HIV-prevention strategies.
Still, challenges remain. The rollout depends on obtaining regulatory approvals, securing timely procurement, and maintaining robust health system capacity to deliver injections every six months. Critics have also raised concerns about geographic limitations: while 120 low- and middle-income countries are covered, some middle-income nations that still carry significant HIV burdens may be excluded. Activists argue that equitable access should be prioritized to prevent widening global disparities in HIV prevention. Financing, training for healthcare workers, and community engagement will also be crucial to ensuring that lenacapavir reaches populations at highest risk.
Lenacapavir represents a unique dual-use medicine; it is already approved for treatment in combination therapy for people with multidrug-resistant HIV, and now its preventive potential is being realized. For prevention, countries adopting the drug will need new clinical guidelines, reliable supply chains, and awareness campaigns to encourage uptake. Experts caution that even as prevention tools improve, systems for HIV testing, treatment initiation, and follow-up remain essential to ensure that people who do contract HIV are not left behind.
If the 2027 timeline and $40 target price are achieved, lenacapavir could revolutionize the landscape of HIV prevention. By overcoming long-standing barriers of adherence, stigma, and affordability, it could help reduce infections on a population scale. Yet, as advocates stress, the true impact will depend on sustained political will, funding commitments, and an unwavering focus on equity. The coming years will determine whether this promising breakthrough becomes the turning point in the decades-long fight against HIV.